Connecting the Dots
Thirty years ago, Stephen Morse MS’74, PhD’77 put a name to the phenomenon that defines our time: emerging viruses.
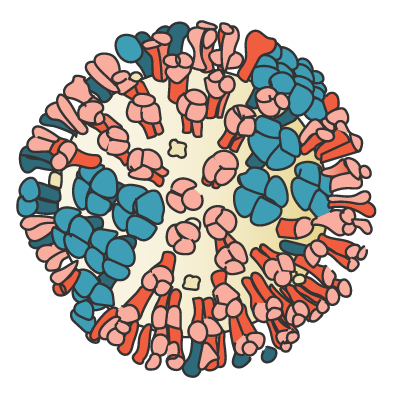
Viruses can acquire their names for their microscopic looks or for the damage they do, or sometimes both, as in the name of the novel coronavirus: SARS-CoV-2 bears a crown (a corona) of spiky protein and inflicts a severe acute respiratory syndrome.
An old convention tagged viruses for the place they were first detected. In 1960, a four-year-old died with a mysterious encephalitis at what is now Gundersen Lutheran Medical Center. UW researchers studying her brain tissue discovered the cause, and named it the La Crosse virus. In the next decades, a rash of viruses moved from their namesake territories and into the news: Ebola virus, named after a river in central Africa where the earliest outbreaks of the deadly hemorrhagic fever occurred; the gut-wrenching norovirus, discovered among schoolchildren in Norwalk, Ohio; hantavirus, isolated from mice along Korea’s Hantan River after outbreaks of another hemorrhagic fever. Then came the 1981 appearance of AIDS.
Timeline
- 1947
Joshua Lederberg joins the faculty at the University of Wisconsin. - 1958
Lederberg wins the Nobel Prize in Physiology or Medicine. - 1971
Stephen Morse arrives in graduate school at the UW. - 1976
Ebola is first identified. - 1981
The CDC first notes an illness it will later call acquired immunodeficiency syndrome, or AIDS. - 1989
Morse organizes the Conference on Emerging Viruses for the National Institutes of Allergy and Infectious Disease. - 1993
Morse edits the book Emerging Viruses. - 1993
Morse helps create ProMED, an online network that monitors emerging diseases. - 1996
Morse heads the biodefense area for the U.S. Department of Defense’s Defense Advanced Research Projects Agency. - 2003
SARS-CoV-1, the first SARS outbreak, is identified; the virus sickens more than 8,000 people. - 2009
H1N1/09 is discovered; it causes the 2009 swine flue pandemic, and as many as 284,000 people die worldwide. - 2012
MERS-CoV (the Middle East respiratory syndrome coronavirus) is first identified. - 2019
SARS-CoV-2, which results in the COVID-19 pandemic, is first identified.
John Allen
In 1988, virologist Stephen Morse MS’74, PhD’77 noticed something important about the constellation of outbreaks. They were all the result of what he called emerging viruses. Instead of just publishing his synthesis in a scientific journal, he found a way to get word out about what it meant for public health. He helped orchestrate a national conference of life-science rock stars — including two Wisconsin Nobel laureates — to put their heads together about not just the HIV/AIDS epidemic that defined the decade, but also what was behind the increasing circulation of viruses around the world.
The landmark conference catalyzed new thinking and action on infectious diseases, especially for Morse, now a professor of epidemiology at Columbia University. “I thought I’d spend all my life working in the lab, as most normal virologists do,” he says.
While he did run a basic-research virus lab, Morse also became an expert in epidemiology. “[Virology and epidemiology] are quite different and demanding fields, and it takes a special scientist to master both,” says his former student Joel Blankson, now a professor at Johns Hopkins University.
Morse has worked with national and international organizations to address what scientists are learning about the changing nature of infectious diseases. He has played key roles on initiatives for the National Academy of Sciences Institute of Medicine, the U.S. Agency for International Development, the global nonprofit Program for Monitoring Emerging Diseases (ProMED), and the Defense Advanced Research Projects Agency (DARPA) at the U.S. Department of Defense, among others.
Morse’s work “has been enormously valuable” in raising awareness among the biomedical community and the public about new infectious diseases and “why it’s important that we recognize and deal with them early,” says Thomas Yuill MS’62, PhD’64, UW professor emeritus of pathobiological science and forestry and wildlife ecology. “COVID-19 is an example of what happens when you don’t.”
FOR HIS WORK ON EMERGING VIRUSES, Morse says, “I will have to give the blame or credit to Josh Lederberg.” He doesn’t recall their first conversation, but he remembers the first close encounter: he found Lederberg’s signature on the borrower’s card of a book he was about to check out from Steenbock Library. Morse was a graduate student in bacteriology, Lederberg a scientific giant who had launched the UW’s Department of Medical Genetics in 1957. In 1958, at age 33, Lederberg shared in a Nobel prize for foundational work in bacterial genetics, then went on to organize the genetics department at Stanford.
Lederberg had been the last person to check out the book on medical statistics. Morse doesn’t remember why he was looking at it. For the bookish, inquisitive kid, it might have been plain curiosity.

Morse says COVID-19 pushed technological developments forward that will better prepare us for the next pandemic. Columbia University
Morse showed up for grad school as a 19-year old, having sped through the City College of New York after graduating from the Bronx High School of Science. He picked the UW sight unseen for its reputation in microbiology, he says, the field he knew he wanted to pursue. A lot of his Sputnik-era youth was spent at the Bronx Zoo and the American Museum of Natural History, where his artist mother worked as a scientific illustrator. His father, who contracted malaria in the South Pacific during World War II, died when Morse was a toddler.
He arrived on campus at a particularly active time in virus research. In veterinary science, Virginia Hinshaw found that human influenza virus (named from the Italian word for influence, reflecting the medieval belief that stars and planets influenced who came down with the seasonal illness) roosts in wild ducks, while Bernard Easterday MS’58, PhD’61 was finding it in domesticated birds and pigs, improving understanding of why the shape-shifting virus is a special scourge. In the medical school, Gabriele Zu Rhein and collaborators discovered the brain-infecting JC virus (named with the initials of the first patient identified with it). Entomology professor Gene DeFoliart, virologist Robert Hanson MS’47, PhD’49, and coworkers had recently found that a woodland mosquito transmits the La Crosse virus, and together with Yuill’s group, the researchers puzzled out that, surprisingly, it endures Wisconsin winters encased in mosquito eggs. And in the McArdle Laboratory, Howard Temin’s research on cancer-causing viruses was about to raise the roof. “It was a remarkable time of discovery,” says Morse.
Morse's work "has been enormously valuable" in raising awareness among the biomedical community and the public about new infectious diseases and "why it's important that we recognize and deal with them early. COVID-19 is an example of what happens when you don't."
He found his niche in Hanson’s lab in veterinary science, where he was steeped in the veterinary concept of “one medicine” and Hanson’s ecology-connected view of animal diseases, ideas that would influence Morse’s future work on emerging viruses. Morse took on the formidable challenge of trying to find the cause of a deadly brain disease in mink; something similar would later emerge as mad cow disease in the United Kingdom and chronic wasting disease in Wisconsin deer. (“I was hoping to discover a new form of life,” Morse says. “I have to confess I didn’t.”)
For his minor in physiological chemistry, Morse also worked at the newly built Waisman Center with neurochemist Steven Kornguth MS’59, PhD’61, who was a role model for “how to be a good scientist and a good person.” Trained in the new molecular biology as well as classical methods of microbiology and virology, Morse landed a couple of east coast virology jobs before circling back home to New York City to research an unusual mouse herpesvirus at Rockefeller University.
LEDERBERG WAS THEN SERVING as Rockefeller’s president, and he still ran a molecular genetics lab. A chance conversation with him steered Morse toward planning the 1989 conference and ultimately a career focused on emerging viruses.
Morse was leaving a 1987 faculty holiday party hosted by Lederberg and his wife, Marguerite, when she reminded Lederberg of something she knew he was concerned about. In Europe and elsewhere, hantavirus was turning up in laboratory rats. Lederberg wondered if lab staff might be at risk from the rodent-borne virus, and he asked the virologist about it as he was getting his coat on.
Morse didn’t know much about hantaviruses, but Lederberg’s query hit its mark. Morse was off and researching, and weeks later he sent his boss a two-page letter about the health concerns of what he called “emerging viruses” like hantavirus. Lederberg responded “in Olympian fashion,” says Morse, who still has the oracular memo: We need some high level policy attention to what needs to be done globally to deal with the threat of emerging viruses.
Morse took it on as another challenge: how to get presidential-level action on the problem. He helped secure sponsors, mainly the National Institute of Allergy and Infectious Diseases, for a conference held at the Hotel Washington in the nation’s capital. With Morse’s name and Lederberg’s conjoined once again, the two scientists opened the two-day May 1989 meeting titled Emerging Viruses: The Evolution of Viruses and Viral Diseases.
Some 200 attendees came for the roster filled with experts such as Temin, who spoke on the conference’s main focus: did new diseases erupt because of rapid viral mutations or new environmental conditions? It was also Temin who advised Morse in follow-up publications to go beyond the naming and define exactly what an emerging virus is.
 Temin’s definition of a virus was “a small genetic system that attaches to cells.” When the coronavirus attaches to cells in the human nose, for example, its genetic system takes over and produces what may be thousands of new virus particles that exit the cell to attach to more cells. Some viruses just hang out superficially in animals, like influenza in ducks and coronaviruses in bats, never becoming systemic infections. But these zoonotic viruses can emerge in humans to become dangerous diseases.
Temin’s definition of a virus was “a small genetic system that attaches to cells.” When the coronavirus attaches to cells in the human nose, for example, its genetic system takes over and produces what may be thousands of new virus particles that exit the cell to attach to more cells. Some viruses just hang out superficially in animals, like influenza in ducks and coronaviruses in bats, never becoming systemic infections. But these zoonotic viruses can emerge in humans to become dangerous diseases.
Morse took General Virology with Howard Temin in 1972 and remembers the teacher as much for his kindness as his brilliance. Temin shared the 1975 Nobel Prize for discovering the enzyme that allows certain RNA viruses to replicate and infect. The enzyme, reverse transcriptase, is the first molecular ingredient in the gold-standard RT-PCR test for COVID-19.
What was changing, Morse and other scientists came to realize, was not so much each virus but rather the conditions a virus could exploit in the larger world. Viral DNA and RNA have been attaching to and shaping humanity from the start, circulating as far as we could go on foot. But with the pace and extent of travel increasing, viruses were now circulating globally. And the myriad viral genetic systems associated with insects and other animals were bound to collide with the increasing number of people building roads and homes in once-forested areas, converting more wildland for agriculture, and seeking bushmeat. Climate change has only upped the odds as it rearranges where plants and animals live.
The 1989 conference highlighted filamentous-like filoviruses such as Ebola; HIV and other retroviruses; and bunyaviruses such as hantavirus and La Crosse — but not coronaviruses. The 1993 book Emerging Viruses that resulted from the conference didn’t discuss them either. For Morse, this proves the point. “Most emerging viruses are surprises,” he says. He defines an emerging virus as one that happens to appear suddenly in a human population and increases rapidly in a region or population.
What was needed, the conference concluded, were early warning systems to discover emerging viruses and ensure a public health response.
IN EARLY JANUARY 2020, virologists began to take note of a cluster of pneumonia-like cases in Wuhan, China. The chatter started after ProMED first reported the cluster on December 30, 2019. ProMED’s moderated digest of news about disease outbreaks was the first such early warning system, and it remains required reading for infectious disease specialists. Instead of relying on slow-acting governments or scientific journals to report outbreaks long after the fact, ProMED checks news sources and specialists from around the world to compile reliable and current information about infectious diseases, whether in people, animals, or plants.
As he did for the emerging viruses conference, Morse played a key role in ProMED’s 1994 launch, as chair of the founding steering committee. He credits Lederberg again for the vision to use what was then an emerging technology — email — to alert infectious disease specialists about outbreaks. What started with 40 subscribers has grown to 87,000, according to Yuill, one of ProMED’s volunteer moderators.
Other early warning systems and fortifications have gone up in the decades since the 1989 conference to prepare for emerging diseases. After the first SARS virus emerged, in 2002, scientists began to warn specifically about new coronaviruses, including in a 2007 paper that referred to a SARS-related “time bomb.” In an October 2019 simulation, Johns Hopkins University went so far as to model what would happen in the event of another coronavirus outbreak, shortly before the novel one, still unknown, would attach itself to human cells in real-life Wuhan.
Why 30 years of scientific evidence and advice about emerging viruses went unheeded in January 2020 is another story.
THE WORDS MORSE USES TO DESCRIBE his reaction to the pandemic sound like stages of grief. Like a seasoned firefighter who has been hearing alarm bells for decades, from AIDS to Zika, Morse at first was “perplexed” by the lack of coordinated response to early reports of the disease. Then he found it “discouraging,” “frustrating,” and finally “heartbreaking” when it became obvious that the little outbreaks everywhere were turning into a global inferno.
“Inevitably there would have been some spread,” he says, but “we could have done much more to stop it.”
Morse points to islands like New Zealand and Taiwan, as well as South Korea and Vietnam, which kept their numbers of COVID-19 cases and deaths low and their economies working. “They did this by the traditional test and trace,” he says. “They acted early and they took it seriously.”
Morse stayed home as waves of cases surged and resurged. “Now I teach about emerging infectious diseases by Zoom in the middle of a pandemic,” he said last winter. “At least it has relevance.”
But amid the grief, he finds light in what scientists have accomplished in an astonishingly short time: identifying existing drugs that can ease the course of COVID-19; developing faster and varied coronavirus tests; clarifying how virus particles transmit in different sizes of airborne drops; using computer modeling and viral genome sequencing to understand how the coronavirus is circulating; even advancing masking from a 101- to a graduate-level science. And offering a bouquet of vaccines now blooming in billions of immune systems.
“That terrible dark cloud gave us silver linings,” Morse says. COVID-19 “pushed these technological developments forward,” and will better prepare us for the next pandemic. •
Christine Mlot ’83 wrote about dining at the UW French House in the Winter 2004 On Wisconsin.
Published in the Fall 2021 issue

Comments
No comments posted yet.