Pain Relievers
A UW group wages a global battle to help desperate cancer patients.
Five years ago, Eva Duarte started the only palliative care hospital unit for adult cancer patients in her native Guatemala.
But in the beginning, she had little to offer them. The country’s strict and complicated drug laws made it practically impossible to fill the prescriptions that Duarte wrote — despite the condition of her patients, more than half of whom were admitted with a diagnosis of advanced cancer and in need of skilled pain management.
“I began from zero,” Duarte says.
The situation is not unusual. When the battle against cancer is all but lost, the journey to the end of life brings pain. In many countries, doctors don’t have access to inexpensive drugs such as morphine that can safely ease that suffering. Or they don’t prescribe morphine, fearing scrutiny and punishment from regulatory authorities that view it as no different from heroin, since both are in the same class of pharmacological drugs called opioids. Their patients come to believe that nothing more can be done, and, in time, only death brings an end to their agony.
The World Health Organization (WHO) estimates that 5.5 million people with terminal cancer and another million in the late stages of HIV/AIDS are not getting the pain relief that they desperately need.
Duarte has an ally at UW-Madison in the Pain & Policy Studies Group, which for fifteen years has worked to elevate pain relief as a human right and has been designated a WHO Collaborating Center for Policy and Communications in Cancer Care. The team of doctors and policy experts, located in the Carbone Cancer Center, works side-by-side with doctors, pharmacists, and health officials who are fighting to change laws and practices in their home countries.
David Joranson ’68, MS’70, the group’s founder and retired director, calls its work “the Wisconsin Idea gone global.” In his travels, he has visited cancer hospitals where pain is ignored, doctors walk past suffering patients, and those in the worst agony are placed in what’s called a “screaming room.” In Georgia, once part of the Soviet Union, patients discharged from the hospital are required to obtain their medications from a local police station.
This worldwide lack of pain relief for terminal cancer patients is so severe that Human Rights Watch issued a report on the problem last year. Some of the countries highlighted in the report specifically for improving morphine access — India, Vietnam, and Romania — were helped by the UW experts to bridge the gap between health care providers and the authorities in charge of drug control.
“We work with countries and governments to say, ‘Hey, it’s a triangle. You actually need educated clinicians who can give the drugs, you actually need access to the drugs, and you need laws that permit the use of them,’ ” says James Cleary, director of the WHO collaborating center and UW’s palliative care program. Palliative care doctors work with patients during transitions in treatment, treat their pain, and guide them through end-of-life decisions.
Kindred Spirits

“I began from zero,” says Eva Duarte, a physician in Guatemala, about her early efforts to help cancer patients. Photo: Bryce Richter
The UW organization helps a small group of international fellows — mostly doctors and pharmacists — become champions for change within their own governments and health care systems.
“They know the medical side of it, but they don’t know how to make the link and bridge the gap with governments and regulatory officials in their country,” says Karen Ryan ’89, MA’97, who leads the fellowship program.
Fellows attend an intense five-day training session in Madison, learning about controlled medications, identifying the barriers in their countries’ health care and drug-distribution systems, and developing action plans to break them down. “They’re wide-eyed when they get here,” Ryan says. “It is totally a systemic problem. It’s policy. It’s medical education. It’s drug availability. It’s cost of medicines.”
To spend any time with the fellows is to see courage and the drive to make a difference. They are dynamic and intelligent people from every corner of the world who have found kindred spirits with one another and their UW mentors. What they share is a huge anchor, because their mission can be lonely work. Along the way, any number of factors — including national elections that bring about massive turnover in the very government agents with whom they work — can stall progress. When the fellows meet face-to-face, usually once a year, the gatherings generate light-bulb moments as they learn about strategies others have used that might work in their own countries.
“It was a relief to know that we were all fighting for the same thing,” says Marta León, a doctor from Bogotá, Colombia, who became a fellow in 2006.
Competition is fierce for those wanting to join the program. For the most recent class of fellows, forty-five applicants were vying for slots eventually filled by eight people from six countries. The UW program evaluates an applicant’s experience, involvement in national palliative care organizations, contacts with government officials, and English skills. The fellowship is open to health care administrators, policy experts, social workers, attorneys, and regulators who want to improve access to pain-relief drugs and palliative care.
For those not admitted to the program, staff members have developed an online course that provides a framework of international and national drug regulation. More than two hundred participants from sixty-six countries have registered for the course.
Smart Battles
The support from the UW and the other fellows gives Duarte, who is one of just four palliative care doctors in Guatemala, the tools to educate others about pain and palliative care. Attitudes in her country dictate that people with cancer should endure chemotherapy until the day before they die, she says.
For three years, before becoming a fellow in 2008, Duarte fought on her own to improve access to morphine and other medical narcotics. “It was like chasing [something] … I didn’t have a plan,” she says. The UW program, she says, taught her how to fight “smart battles.”
“It was very nice to be a superhero sometimes, but not being the only superhero,” Duarte says. “It took me out of that place of frustration and isolation, because I was so alone in fighting things and even wondering, ‘Am I right or wrong?’ ”
Her first step was identifying the barriers blocking access to affordable drugs. Low-cost oral morphine was not available in Guatemala. The only opioid medicines available were very expensive, costing more than a day’s salary. Pharmacies could only fill prescriptions approved by a government agency that has just one office for the entire country. Depending on where patients live, Duarte says, “this could take some minutes, this could take some hours, this could take some days” — and that’s if the pharmacies agreed to handle the prescription at all.
After Duarte’s first session in Wisconsin, she made progress, winning government approval for her hospital to use an internal, pre-authorized prescription form for medications, rather than the original exhaustive authentication process. However, she says, getting morphine is still difficult, although it’s now on the list of medications covered by the country’s national health plan. And she’s still working with the ministry of health and drug regulators to implement an electronic approval system for prescriptions.
“We have a wall that is blocking the happy ending,” she says.

“It was a relief to know that we were all fighting for the same thing,” says Marta León, a physician in Colombia. Bryce Richter
Finding Balance
Nearly fifty years ago, countries enacted an international treaty to stem the production and supply of narcotic drugs. The treaty, now signed by 184 nations, also states that such drugs are essential for the relief of pain and suffering, and that governments are obligated to make them available for medical treatment and research.
Yet the day-to-day reality for cancer patients in more than one hundred countries is pain. Fear and stigma surrounding narcotic drugs have gotten in the way of pain relief. That’s due to the long-standing myth that taking morphine for medical purposes automatically leads to addiction, and to the lack of education for many doctors about how to properly use the drugs. In fact, only in recent years has the United Nations Office on Drugs and Crime issued statements to countries that encourage access to pain-relieving narcotics for patients who need them.
In the 1990s, the UW group began collaborating with WHO to address the lack of access to pain medicines. They developed guidelines for evaluating a country’s drug-control policies, starting with the principle that a nation’s drug laws should strike a balance between ensuring that drugs are available for pain relief and preventing their abuse and trafficking.
It sounds easier than it is.
“When I’m doing these workshops with people in different countries, I ask, ‘How do you say balance in your language?’ — and you get some pretty interesting responses,” says Joranson, the UW group’s founder. “There’s a lot of discussion, first of all, to define [balance] correctly, and then they try to find the right word.”
The UW team is mindful that diversion of morphine or other narcotics intended for medical use can derail efforts to improve access.
“That’s a sure way to take three steps backward,” Ryan tells the fellows during an August training and strategy session in Madison. “We don’t want the pendulum to swing so far. … We don’t want them to fall into the wrong hands.”
Supply and Demand
In India, the laws covering the use and distribution of drugs are complex. They fill a 1,389-page book, as thick as the six-inch binder that Joranson bought at a Delhi bookstore. The mammoth volume is an intimidating reminder of what’s keeping pain relief from patients.
After India broke free of British rule in 1947, twenty-eight states came together and adopted a constitution that allowed each of them to individually control drug regulation. To move a narcotic drug from one state to another requires an import permit, an export permit, and a transport permit. Think red tape.
“If you’re in one state and you want to get morphine out of a government factory, you have to get two states involved in transferring every consignment,” Joranson says.
Even Indian doctor R.B. Ghooi struggled in vain to find pain-relieving drugs for his mother, who died of cancer in 1997. From government officials and bureaucrats, Ghooi wrote, he “received tons of sympathy — but not a milligram of morphine.”
So why not just increase the supply of morphine to meet the demand? It turns out that supply isn’t the problem; there’s already more than enough to go around. Forty percent of the world’s legal poppy crop is grown in Tasmania, with other major growing areas in Turkey and India.
The International Narcotics Control Board tightly regulates all of these areas.
Growing more poppies won’t erase the challenges in countries where people die in pain. While India supplies much of the opium to make morphine for use in the rest of the world, it produces very little for its own use because of low demand. Twice during the 1990s, the Indian government used funds to purchase a large lot of oral morphine to distribute to regional cancer centers. “They ran into the same problems that we were trying to straighten out, and most of the morphine was never distributed and ultimately was wasted,” Joranson says. “They were trying to come up with a simple supply-side solution to what is really an infrastructure and a demand-side problem.”
Joranson has spent a lot of time on planes and trains in India with M.R. Rajagopal, who is considered the father of palliative care in that country, traveling to different states to work with cancer doctors and government officials to improve access. Fourteen of twenty-eight states have adopted a simplified rule governing narcotics, which Joranson first recommended in 1998. Rajagopal says the work of Joranson and others at the UW “has had such a huge impact on the pain burden in the world.”
How much morphine a country can purchase for medical use is based on an estimate that governments submit to the International Narcotics Control Board. Some countries submit no estimates at all or request enough to help only a handful of patients; others miss the mark by submitting an estimate based on the previous year’s consumption, which wasn’t enough.
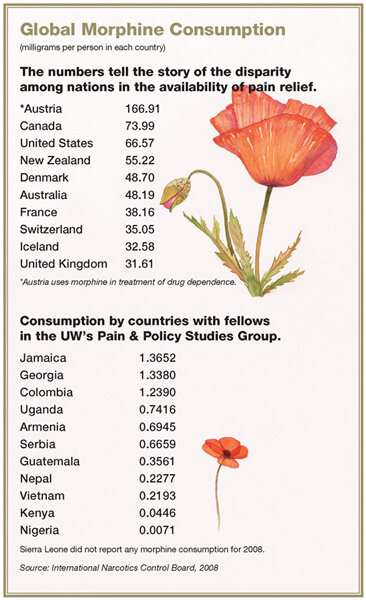
Statistics for morphine consumption in milligrams per person by country tell the story. The UW’s Cleary says there is essentially a “thousands-fold difference” between developed and undeveloped countries. While the United States consumes nearly 67 milligrams of morphine per person each year, Ethiopia sits at the other end of the spectrum, with .0045 milligrams per person.
“So there’s no pain relief in terms of morphine,” Cleary says.
Improving estimates, physician education, and public awareness are all keys to developing better pain relief in affected countries. Ryan and her UW colleagues are working with the narcotics control board to refine how governments are instructed to calculate estimated needs for morphine and other pain-relieving medications.
“Sometimes it’s a weak demand that leads to inadequate supply. Sometimes it’s a failure of the government to accurately assess its needs, but it’s the kind of a problem that can only be solved by people working together in the country,” Joranson says.
No Pain After Five O’Clock?
Morphine was available in Bogotá, where the government produces it, when Marta León first joined the fellows program. But she found a very different story outside Colombia’s capital city when she surveyed regulators and health care providers about drug availability in their regions of the country.
“Every time we heard the same [thing]: sometimes they will have one opioid for a while, and then they won’t have any for a couple of months,” says León, a doctor who heads the pain and palliative care department at Universidad de La Sabana.
Pharmacies throughout Colombia that stocked opioids had very limited hours. “They would have a very strange schedule — 8 to 5, Monday through Friday. So [apparently] it was impossible for you to have pain during the weekend or at night,” she says.
Two years ago, a local newspaper ran a classified ad on behalf of a thirty-six-year-old woman with advanced cancer who lived nearly three hundred miles from Bogotá. It was a cry for help: “Cancer is killing us. Pain is killing me because for several days I have not been able to find injectable morphine in any place. Please, Mr. Secretary of Health, do not make us suffer anymore.”
In 2007, León brought together in one room everyone who played a part in the chain of distribution: representatives of the Ministry of Health, the national and state authorities, pain and palliative care physicians, and international leaders in the efforts, including Joranson and Ryan. Today, because of the work of Le√≥n and drug regulators, each state has at least one pharmacy that dispenses opioids open around the clock, seven days a week.
In spite of this progress, there are other problems. It has become clear to León that she also needs to work with the departments of health in each of Colombia’s thirty-two states (which she refers to as “thirty-two problems”) and with the country’s version of HMOs to ensure an ongoing, reliable supply of medications from Bogotá to other regions of the country. The obstacles still preventing patient access to pain relief in Colombia reflect the depth of the systemic barriers found throughout the world.
Addiction Myth
Pain — and how to manage it — has been wildly misunderstood. Experts in the field say that some of the push for physician-assisted suicide, in fact, stems from poor pain control.
In 1984, some members of the U.S. Congress proposed making heroin legal for people dying from cancer. Joranson was then serving as administrator of Wisconsin’s Controlled Substances Board, where he had developed an approach to identify doctors who were abusing their prescriptive privileges. The proposal to make heroin legal prompted Joranson to join forces with June Dahl, another board member and a UW pharmacology professor. They investigated what was driving the unexpected proposal.
“[They] had some crazy idea that heroin was a magic bullet,” says Dahl, former director of the Alliance of State Pain Initiatives, a U.S. network of groups
dedicated to promoting pain relief. “It’s not. It’s an expensive, controversial way to give morphine, because it’s converted to morphine in the body.”
Dahl and Joranson launched the Wisconsin Cancer Pain Initiative, aimed at educating physicians and reforming regulations to improve care. Their efforts garnered attention from the Oxford Textbook of Palliative Care, which calls the Wisconsin initiative “pioneering.”
Dahl and Joranson concluded that the problem wasn’t a shortage of drugs. Instead, Dahl says, “[the drugs] weren’t being used appropriately and people had the wrong attitude. They were terrified of addiction.”
People who use morphine to relieve pain can become physically dependent on the drug and even go through withdrawal, but that doesn’t mean they are addicted. That bears repeating: addiction and physical dependence are not the same thing. Addiction results in the compulsive use of drugs despite harm, and evidence shows it is not more common in patients with chronic pain from cancer than in the general population.
Yet, for decades, medical texts and laws stated that addiction was to be measured by withdrawal symptoms, which led to doctors confusing the appropriate treatment of pain with addiction. WHO issued a definition of addiction in the 1950s, stating that physical dependence or withdrawal was inevitable for people who used morphine and that it should be avoided.
“You can’t be surprised that people are afraid of using these drugs and making them more available,” Joranson says.
More Than Work
Members of the UW’s Pain & Policy Studies Group have the passport stamps to prove how widely they’ve traveled in their quest to ease pain.
The group receives no money from UW-Madison or WHO. It relies on grants from private organizations, including the Lance Armstrong Foundation, the Susan G. Komen Foundation, the American Cancer Society, and the Open Society Institute founded by George Soros.
“It’s not just work for them,” says Willem Scholten, who leads the access to controlled medicines program for WHO in Geneva. “David [Joranson] has retired now, but he’s still working on the issue. So that makes it quite clear.”
They have seen reasons to hope: physicians who walk through jungles to reach patients who need morphine; countries such as Sierra Leone, where the first hospice can now offer morphine to its patients; government officials and fellows sitting down at the same table in Wisconsin to draft new laws for Romania and Vietnam to replace decades of anti-narcotics regulations.
But the journey is far from over.
As just one reminder, Joranson displays a photo that he took at a hospice in sub-Saharan Africa in 2002. It shows a pristine, white, metal cabinet. The door is hanging open with the keys dangling from the lock, and the word poison — used to refer to pain-relieving drugs in some countries — is painted on the front in English and Dutch. The shelves are empty.
Jenny Price ’96 is senior writer for On Wisconsin.
Published in the Winter 2010 issue


Comments
Frank Ryan November 16, 2010
Heckuva job, Jenny. Karen Ryan is one of my favorite daughters-in-law, by the way. Smart, compassionate, hard-worker…just like her father-in-law. Keep up the good fight. Frank Ryan, Middleton, WI
Dr. R. B. Ghooi November 22, 2010
Excellent article, very well researched and well written. Twelve years after my mother, my wife died of cancer barely two months ago. In 1998, with the help of David Joranson, and Dr. MR Rajagopal, we filed a Public Interest Litigation in Delhi High Court, and won it. The court ordered the governments to modify laws so as to enable every patient free access to opioids. Unfortunately only 11 of the 28 states did so and now we are back in the Supreme Court of India fighting for change of rules all over the country.
Little did I know in 1998 that our struggle will help me when I needed morphine for my wife. Cipla’s Palliative Care Center Pune made morphine available for her without any red tape or delays.
I would like to become a Fellow of your program, I will talk to David about it.
Thanks for your thoughtful article, I hope it gets widely publicized and read.
Ravi Ghooi
Sue Ann Hubanks December 7, 2010
Wow! I am totally amazed with people such as Eva Duarte, Karen Ryan, Marta Leon, David Joranson and Dr. Ghooi. Their tenacity and selflessness is unmatched. They ‘speak’ for those who cannot. The organizations such as Pain and Policy Studies Group, UW Carbone Cancer Center and WHO are also advocates for those without voice….keep up the wonderful work!
Neil McPhail December 30, 2010
great article I have a question.
Local mortician states when us embalming fluid a distinct odor is given off when embalmed has been on methadone is there a corelation between methadone and embalming fluid to give an odor from interaction of the two substances? If have sources for answer please send.
Thank you in advance,
Neil McPhail BS RPh
Stacy April 21, 2011
Fantastic, well researched & written article. Great job!
Joe June 12, 2012
Thank you. As a pharmacist learning about pain this helps!